Kratom, from the Mitragyna speciosa plant, has gained attention as a natural alternative for chronic pain management due to its alkaloids, mitragynine and 7-hydroxymitragynine, which engage with opioid receptors. These compounds influence neurological pathways associated with pain and offer an analgesic effect without the typical sedation or respiratory risks seen with traditional opioids. While it presents a non-addictive option for pain relief, it's crucial to consult healthcare providers due to individual differences in response and potential interactions with other substances. The efficacy and safety of kratom in chronic pain management are under ongoing scientific scrutiny to ensure its responsible use. Users should be aware of the varying strains like Maeng Da or Bali, and their different effects, and should adopt a holistic approach that includes proper dosing, diet, hydration, and rest. Regular monitoring of health outcomes is essential when integrating kratom into pain management strategies.
Exploring the potential of kratom as a natural approach in chronic pain management, this article delves into its role in inflammation reduction. Through scientific analysis, we uncover the mechanisms behind kratom’s anti-inflammatory properties and provide guidance on safely incorporating it into your pain relief regimen. Join us as we navigate the intersection of herbal remedies and medical science to alleviate persistent discomfort.
- Understanding Kratom's Role in Chronic Pain Management
- The Science Behind Kratom and Inflammation Reduction
- Safely Integrating Kratom into a Pain Management Routine
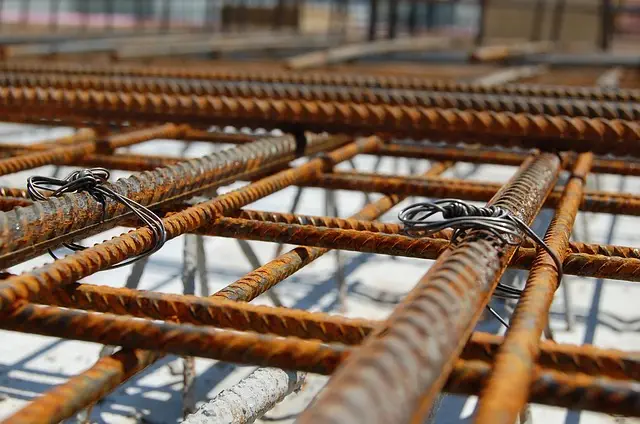
Understanding Kratom's Role in Chronic Pain Management

Kratom, a plant native to Southeast Asia, has garnered attention in the realm of chronic pain management due to its potential therapeutic properties. The leaves of kratom contain alkaloids, primarily mitragynine and 7-hydroxymitragynine, which are believed to interact with the body’s opioid receptors, offering analgesic effects. Users often report relief from chronic pain, a condition characterized by persistent pain that persists beyond the typical healing time. The efficacy of kratom in managing such pain stems from its ability to influence various neurological pathways involved in pain perception and modulation. Research indicates that the alkaloids present in kratom can bind to mu-opioid receptors, similar to opioid drugs, but without the same level of sedation or respiratory depression. This selective interaction is what makes kratom a subject of interest for those seeking alternatives to traditional pain medications, which may come with adverse side effects or addiction risks. It’s important for individuals considering kratom as part of their chronic pain management plan to consult healthcare professionals, as the use of kratom can have varying effects and may not be suitable for everyone due to its potency and potential interactions with other substances. Additionally, ongoing research into the long-term effects of kratom consumption is crucial to fully understand its role in pain management and to ensure safe and effective use within this context.
The Science Behind Kratom and Inflammation Reduction
Studies have indicated that kratom, a plant-based substance derived from the leaves of Mitragyna speciosa, contains alkaloids with potential anti-inflammatory properties. These alkaloids, primarily mitraphylline and 7-hydroxymitragynine, are thought to interact with the body’s opioid receptors, thereby modulating pain signals and potentially reducing inflammation. The scientific rationale behind kratom’s anti-inflammatory effects is rooted in its ability to influence several cellular signaling pathways that regulate immune responses and inflammation. Preclinical research has shown that kratom can inhibit the activation of nuclear factor kappa B (NF-κB), a key transcription factor involved in the regulation of genes associated with inflammation, suggesting a plausible mechanism for its anti-inflammatory actions. Additionally, the alkaloids found in kratom may also influence other immune system components such as cytokines and enzymes that play critical roles in both acute and chronic inflammation. As a result, kratom holds promise as a natural approach for chronic pain management, offering an alternative to conventional nonsteroidal anti-inflammatory drugs (NSAIDs) for those suffering from conditions characterized by persistent inflammatory responses. However, it is imperative that further scientific investigation be conducted to fully understand the scope and efficacy of kratom in inflammation reduction, considering the complexity of inflammatory processes and individual differences in response to such substances.
Safely Integrating Kratom into a Pain Management Routine
When considering chronic pain management strategies, individuals often explore alternative solutions that offer both relief and safety. Kratom, a plant from Southeast Asia with alkaloids that interact with opioid receptors in the brain, has emerged as a potential natural supplement for managing such pain. To safely integrate kratom into a pain management routine, it is crucial to approach its use with caution and informed decision-making. Beginning with small, measured doses is pivotal to gauge individual tolerance and effects. It is also essential to maintain open communication with healthcare providers, as kratom can interact with other medications and may not be suitable for everyone due to personal health conditions or concurrent treatments.
Moreover, adhering to a regimen that includes proper diet, hydration, and rest is essential when incorporating kratom into daily life. The choice of kratom strain also plays a significant role; some strains may be more effective for pain relief than others. Users should educate themselves on the various strains available, such as Maeng Da or Bali, and their potential effects on chronic pain symptoms. It is advisable to consult with knowledgeable professionals who specialize in natural and alternative treatments to tailor a personalized approach that aligns with one’s specific needs and circumstances. Regular monitoring of both physical and psychological well-being is necessary to ensure kratom is used responsibly and effectively for chronic pain management.
Kratom’s potential in chronic pain management, particularly in reducing inflammation, presents an intriguing avenue for those seeking alternative therapies. The scientific evidence supporting its anti-inflammatory effects underscores the need for further research to fully understand its mechanisms and safety profile. As discussed, integrating kratom into a pain management routine should be done with caution and professional guidance to navigate its complexities effectively. It is clear that kratom could play a significant role in the realm of chronic pain management; however, more studies are essential to ensure its responsible use. Potential benefits must be weighed against any adverse effects to provide patients and healthcare providers with comprehensive information for informed decision-making.